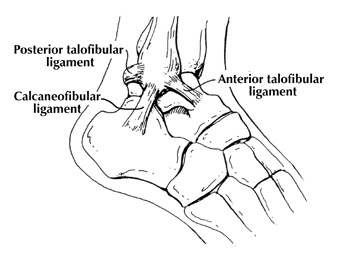
Ankle Instability
The most common way an ankle sprain occurs is when the foot lands on an uneven surface and the foot rolls in (as seen in the picture below). The ligaments are stretched and depending on the severity they may be partially or completely torn.
Pain may be on the inside of the ankle (medial side) due to bruising of the bone and ligament as well as over the area of the damaged ligament/s and muscles on the lateral side.
Core Stability and Back Pain
Pain has been shown to inhibit the core stability muscles, and can also result in the adoption of pain relieving positions which can exacerbate the problem. Core stability provides a focus, both mental and physical, away from symptomatic relief and towards constructive support of the painful structures. Improving core stability and postural awareness can sometimes produce instant relief.
However, a slow reduction in pain, requiring some commitment from the patient is more common. Pain may be on the inside of the ankle (medial side) due to bruising of the bone and ligament as well as over the area of the damaged ligament/s and muscles on the lateral side.
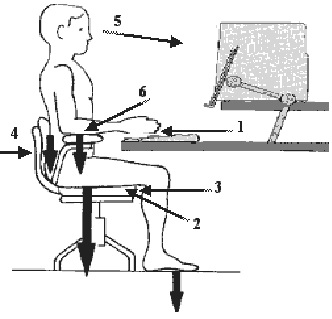
Ergonomic Office Setup
1) Provide good even lighting
2) Give yourself plenty of desktop space
3) Control unwanted noise
4) Arrange your storage sensibly
5) Provide heating and cooling
6) Correctly set-up your office chair – when purchasing a new office chair, ensure it:
– Has an adjustable low back support
– Is adjustable in height
– Is stable – ideally a five star base
Imagery and Chronic Pain Control Techniques
The important role the mind plays in chronic pain is clearly recognized in the medical literature, as well as in the International Association for the Study of Pain’s definition of pain, which states that ‘pain is always subjective and is defined by the person who experiences it’.
The consequence is that the brain can also learn how to manage the sensation of pain. Using the mind to control chronic pain, or the use of coping strategies for managing persistent pain, may be used alone or in tandem with other pain management therapies.
Ideally, use of the chronic pain management techniques outlined in this information sheet can help patients feel less dependent on painkillers and feel more empowered to be able to control their pain.
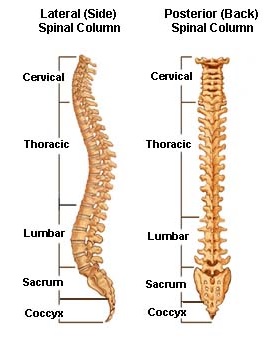
Lumbar Facet Joint Pain
Common Causes of Facet Joint Pain:
• Repetive extension movements or prolonged periods of extension of the lumbar spine
• Poor standing and sitting postures for prolonged periods
• Weak stabilizing muscles leading to increased stress on the facet joints
Persistant Pain
Pain is an ‘unpleasant sensory and emotional experience associated with actual or potential tissue damage’. Acute pain commonly lasts for less than 30 days, whilst chronic pain has a duration of more than three to six months. However a more appropriate definition of chronic pain is ‘pain that extends beyond the expected period of healing’. Most commonly pain occurs when your body’s ‘alarm’ system alerts the brain to actual or potential damage. Pain makes you move differently, think differently and behave differently.
Physio For You – Diabetes and Lymphoedema
Diabetes is a condition where the body is unable to automatically regulate blood glucose levels, resulting in too much glucose (a sugar) in the blood.
Lymphoedema is characterised by swelling of certain parts of the body, caused by problems with the lymphatic system. The lymphatic system is a network of tubes throughout the body that drains this fluid (called lymph) from tissues and empties it back into the bloodstream. Normally, fluid and proteins leak into the body tissues regularly from the blood. This tissue fluid bathes the cells, supplies their nutritional needs and receives back the products of this chemical process. When this system is not working properly, lymphoedema can occur.
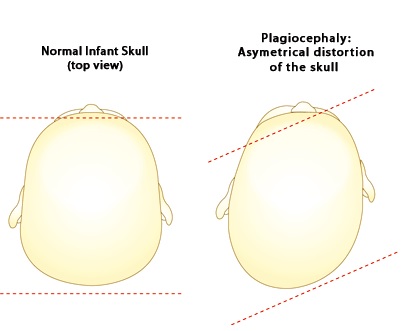
Plagiocephaly
Signs and Symptoms
– Flattening of the back of the skull
– A prominent forehead and fuller cheek on the affected side
– A parallelogram shaped head
– Ear on the affected side placed more anterior
Risk Factors
– Assisted delivery
– First-born child
– Male gender
– Over-exposure to lying on their back
– Torticollis – shortening of neck muscles
– Prematurity
– In utero constraint
Causes
– Sleeping on their back
– Torticollis
– Prematurity – softer bones
– Restricted intrauterine environment
Plantar Fasciitis
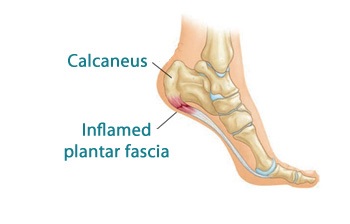
Plantar Fasciitis is the most common form of heel pain. The Plantar Fascia is the flat band of tissue (ligament) that connects your heel bone to your toes, supporting the arch of your foot. Under normal circumstances the plantar fascia acts as a shock absorber, however if the tension on this ligament becomes too great, irritation or inflammation can occur causing pain.
Plantar Fasciitis is inflammation of this ligament, occurring where it inserts into the heel bone. Plantar Fasciitis is most common in middle-aged to older people, with 50% of over 50 year olds developing Plantar Fasciitis. However it can also occur in younger people who are on their feet a lot. Symptoms are a sharp pain in the heel, especially when getting out of bed in the morning. The pain will usually subside but then return after prolonged standing or walking.
Right Sided Torticollis
Torticollis is a condition where a neck muscle called the sternocleidomastoid is shorter on one side of the neck than the other. Torticollis causes your baby’s head to be pulled towards the short muscle and their chin turned away to the opposite side.
The increased pressure on one side of the back of the skull can result in changes to the head shape, a condition known as plagiocephaly. Right-sided torticollis involves a tilt to the right and rotation of the skull to the left, likely to result in a flattened left posterior skull, prominent left cheekbone and left ear.
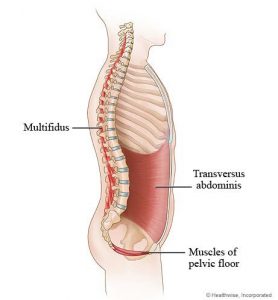
Clinical Pilates and Gym
Clinical pilates focuses on core stability training of the abdomindal muscles that support the spine. The deep muscles of Transverse Abdominus work like a corset around the middle. Multifidis and the Pelvic Floor also help to stabilise and act like a brace to protect the lower back throughout the day.
These muscles hold the vertebrae in the back strong so that there is not too much movement between the vertebrae when the body moves throughout the day to sit, stand, walk, run, lift along with many other daily activities.
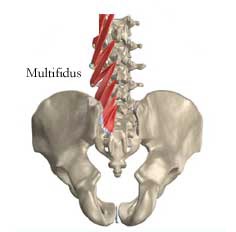
Stabilising exercises for Low Back Pain
Recent research into the causes of persistent low back pain has shown that many sufferers of this common problem have an associated weakness of the muscles surrounding their lumbar spine. The two main muscles that are thought to be involved here are the small multifidus muscles, located behind your vertebrae, and the transversus abdominus muscles, located in front of the vertebrae underneath you abdominal muscles.
Throughout the day, these muscles normally act like a corset or brace around your low back protecting the vertebrae from moving too much on one another – as you sit, walk, run, lift, or do any sort of physical activity. Their action is very subtle and usually occurs without any conscious thought or effort. Contraction of these muscles doesn’t result in any noticeable movement (an isometric co-contraction) – their role is to stabilise your spine – keeping bones, joints and ligaments aligned properly with one another.
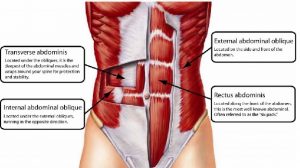
The Abdominal Muscles
The abdominals are located between the ribs and pelvis and act to support the trunk, allow movement and hold organs in place. There are four layers of abdominal muscles, each with a different purpose:
Rectus Abdominus – located between the ribs and pubic bone and the front of the pelvis, the main purpose of this muscle is to allow large movements of bending. This muscle is commonly known as the ‘six-pack’ muscle.
External and Internal Oblique – these muscles are located on each side of the rectus abdominus, and allow the trunk to twist.
Transversus Abdominus (TA) – This muscle is the deepest layer. Its main role is to stabilize the trunk and maintain internal abdominal pressure.
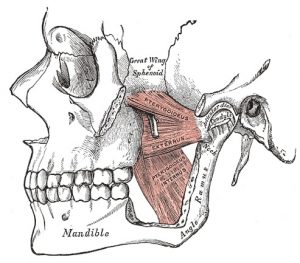
TMJ Disorder
The temporomandibular joint (TMJ) is formed by the mandible or jawbone joining with the temporal bone of the skull, just below and in front of the ear. Each joint has a cartilage disc inside keeping the temporal bones and the mandible bone apart to prevent the bone surfaces from wearing and damaging each other, as well as to act as shock absorber for the joint. The jaw joint is surrounded by a capsule or envelope enclosing it.
The TMJ is opened and closed thousands of times each day as we eat, speak, breath, and yawn, and is thus the focal point of much activity and physical forces. Jaw movement is driven by many muscles connected to the skull and the neck, which are responsible for its different actions. Additionally the muscles involved in keeping the jaw in a rest position have a direct connection to the neck. Therefore in diagnosing a TMJ disorder it is important to look at the neck and areas of the body that may affect the neck.

Vertigo
BPPV, also known as paroxysmal positional vertigo, is a spinning sensation of the head (vertigo) brought on by a certain position of the head, usually sudden changes of position.
The word “benign” means it is not a serious condition and is likely to get better with treatment.
VMO Exercises
“VMO” stands for the Vastus Medialis Oblique muscle. It is part of the large muscle group that sits on the front of the thigh – the quadriceps or “quads”. The VMO runs along the inside for your leg, just above the knee. The action of the VMO is very
important in walking, running and any weight bearing activity that involves bending
of the knee.
As your knee bends and straightens, the patella (knee cap) slides up and down over the end of the thigh bone, or femur. Muscles on either side of the patella contract to help guide this movement. The muscles on the outside edge of the patella pull it towards the outside of the leg. To balance this movement, the VMO muscle pulls the patella towards the inside of the leg.
Treatment duration depends on your diagnosis, the severity of your impairments, your past medical history, and other factors. Re-evaluations will be done to assess your progress and your therapist communicates with your physician to help you achieve your therapy goals.
We sees and treats patient for a wide range of conditions and diagnoses. Please visit our Services for an extensive list of conditions and diagnoses we see patients for.
Physical Therapy at Physio is proud to have 20 physical and occupational therapists on staff who have obtained and achieved advanced certifications in orthopedics, sports, hand therapy, manual therapy, and pedorthics.
We will check with your health insurance provide to determine if outpatient physical therapy services are covered under your plan. We recommend that you confirm your insurance coverage.
Call the facility in which you go to for all your regular appointments. You may also call our administration office at + 123 556 7890.
Ask us a Question
Feel free to ask any physical therapy related questions over the phone, or get send your question via this form below. Your message will be dispatched directly to our staff who will answer as soon as they can.